Understanding Blood Sugar Levels
Blood sugar, also called blood glucose, is the primary fuel your body uses for energy. It comes from the food you eat, and your body controls it with the help of insulin, a hormone made by the pancreas. Maintaining balanced blood sugar levels is essential for good health, as both high and low levels can cause serious problems over time. But what is considered a normal blood sugar level, and when should you start to worry? Understanding these numbers can help you take better care of your health and prevent future complications.
Why Blood Sugar Matters
Your body depends on a steady supply of glucose to keep everything running smoothly. When blood sugar levels are too high or too low, it can lead to serious health problems. Low blood sugar (hypoglycemia) can cause dizziness, confusion, and even fainting, while high blood sugar (hyperglycemia) can damage organs over time.
If left uncontrolled, high blood sugar increases the risk of diabetes, heart disease, nerve damage, and vision loss. That’s why keeping your glucose levels in a healthy range is essential for overall well-being. By understanding how blood sugar affects your body, you can take steps to protect your health and prevent complications.
What Is a Normal Blood Sugar Level?
Blood sugar levels can change throughout the day based on what you eat, how active you are, and even your stress levels. Keeping your glucose within a healthy range helps prevent complications. Here’s a general guide to normal, pre-diabetic, and diabetic blood sugar levels:
- Fasting blood sugar (before eating):
- Normal: 70–99 mg/dL
- Pre-diabetes: 100–125 mg/dL
- Diabetes: 126 mg/dL or higher
- After eating (1-2 hours post-meal):
- Normal: Below 140 mg/dL
- Pre-diabetes: 140–199 mg/dL
- Diabetes: 200 mg/dL or higher
- HbA1c (average blood sugar over 3 months):
- Normal: Below 5.7%
- Pre-diabetes: 5.7–6.4%
- Diabetes: 6.5% or higher
Regular monitoring can help you stay within a healthy range. If your levels are consistently high or low, talk to your doctor about ways to manage your blood sugar and reduce your risk of diabetes-related complications.
Factors That Affect Blood Sugar
Many different factors can influence your blood sugar levels. Understanding these can help you make better choices to keep your glucose in a healthy range.
- Diet – The food you eat plays a major role. Carbohydrates, like bread, pasta, and sweets, raise blood sugar the most. Protein and healthy fats have a smaller impact but can still affect glucose levels.
- Exercise – Physical activity helps lower blood sugar by making your body more sensitive to insulin. Regular movement, like walking or strength training, can help keep your levels stable.
- Stress – When you’re stressed, your body releases hormones like cortisol, which can cause blood sugar to rise. Finding ways to manage stress, such as meditation or deep breathing, can help keep levels in check.
- Sleep – Poor sleep can interfere with insulin function, leading to higher blood sugar. Aim for 7–9 hours of quality sleep each night to support healthy glucose levels.
- Medications – Certain drugs, like steroids, birth control pills, and some antidepressants, can affect blood sugar control. If you’re on medication, talk to your doctor about its impact on your glucose levels.
By understanding these factors, you can take steps to manage your blood sugar and maintain better overall health.
What Causes High Blood Sugar?
High blood sugar (hyperglycemia) occurs when your body doesn’t use insulin properly or doesn’t produce enough of it. This leads to excess glucose in the bloodstream, which can cause health problems over time. Common causes of high blood sugar include:
- Eating too many carbs or sugary foods – Carbohydrates break down into glucose, causing blood sugar levels to rise.
- Lack of physical activity – Exercise helps your body use insulin more efficiently. Without movement, blood sugar can stay high.
- Stress or illness – When you’re stressed or sick, your body releases hormones that can raise blood sugar.
- Insulin resistance – This condition, common in Type 2 diabetes, makes it harder for your body to use insulin effectively.
- Missing diabetes medication – If you have diabetes and skip medication, your blood sugar may rise too high.
- Dehydration – Not drinking enough water can make blood sugar levels more concentrated, leading to higher readings.
Symptoms of High Blood Sugar
If your blood sugar is too high, you may notice:
- Increased thirst
- Frequent urination
- Fatigue
- Blurry vision
- Headaches
- Slow-healing wounds
Long-term high blood sugar can lead to serious complications, including nerve damage, kidney disease, and heart problems. Monitoring your glucose levels and making healthy lifestyle choices can help prevent these risks.dney disease, and heart problems. It can also increase the risk of stroke and infections.
How to Lower High Blood Sugar
If your blood sugar is too high, there are several steps you can take to bring it back to a healthy range. Managing blood sugar levels is important to prevent complications and maintain overall well-being.
- Drink more water – Staying hydrated helps your kidneys flush out excess sugar through urine, lowering blood glucose naturally. Aim to drink plenty of water throughout the day.
- Exercise regularly – Physical activity helps your muscles use glucose for energy, which lowers blood sugar. A brisk walk, strength training, or even simple movements like stretching can make a difference.
- Eat fiber-rich foods – Fiber slows down glucose absorption, preventing spikes in blood sugar. Include foods like whole grains, vegetables, legumes, and nuts in your diet.
- Manage stress – Stress releases hormones that can raise blood sugar levels. Practicing relaxation techniques like meditation, deep breathing, or yoga can help keep your glucose levels stable.
- Take medication as directed – If you have diabetes, following your doctor’s prescription is essential. Skipping doses or taking the wrong amount can lead to uncontrolled blood sugar.
By making these healthy choices, you can help regulate your blood sugar and reduce the risk of diabetes-related complications. If your levels remain high, consult your healthcare provider for further guidance.

What Causes Low Blood Sugar?
Low blood sugar (hypoglycemia) occurs when glucose levels drop below 70 mg/dL. This can happen for several reasons, including:
- Skipping meals – Not eating for long periods can cause blood sugar to fall too low.
- Excessive physical activity without eating enough – Exercise uses up glucose, and without enough food, blood sugar can drop quickly.
- Taking too much insulin or diabetes medication – Overmedicating can cause blood sugar to fall dangerously low.
- Drinking alcohol without food – Alcohol can lower blood sugar, especially if consumed on an empty stomach.
- Certain medical conditions – Disorders affecting the adrenal or pituitary glands can interfere with blood sugar regulation.
Symptoms of Low Blood Sugar
When blood sugar drops too low, you may experience:
- Shakiness or dizziness
- Sweating
- Confusion or difficulty concentrating
- Hunger
- Irritability or mood swings
- Fast heartbeat
Severe hypoglycemia can lead to fainting, seizures, or even coma. That’s why it’s important to recognize and treat low blood sugar quickly.
How to Raise Low Blood Sugar
If your blood sugar is too low, follow the 15-15 Rule:
- Eat 15 grams of fast-acting carbs, such as:
- ½ cup of fruit juice
- 1 tablespoon of honey
- 4 glucose tablets
- Wait 15 minutes, then check your blood sugar again.
- If it’s still low, repeat the process until your levels return to a safe range.
Keeping quick sources of sugar on hand and eating balanced meals can help prevent low blood sugar episodes. If hypoglycemia happens frequently, talk to your doctor about adjusting your diet or medication.
How to Keep Blood Sugar in a Healthy Range
Managing blood sugar is key to preventing diabetes and staying healthy. Here’s how:
1. Eat a Balanced Diet
- Choose whole grains, lean proteins, and healthy fats.
- Avoid refined carbs and sugary drinks.
- Eat plenty of fiber-rich foods like vegetables, beans, and nuts.
- Stick to a consistent meal schedule to prevent spikes and crashes.
2. Stay Active
- Aim for at least 150 minutes of moderate exercise per week.
- Walking, cycling, swimming, or strength training can help regulate blood sugar.
- Avoid long periods of sitting—try to move every 30 minutes.
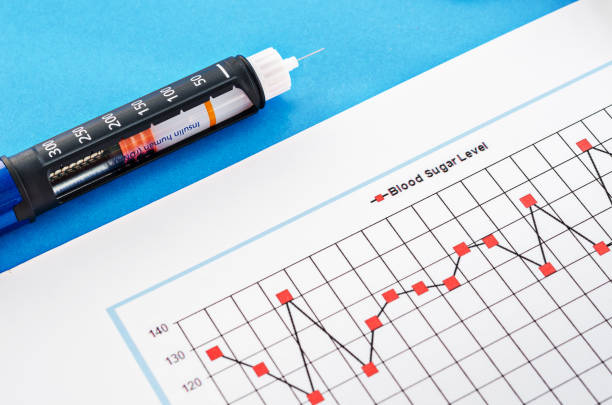
3. Monitor Your Blood Sugar
- If you have diabetes or prediabetes, check your levels regularly.
- Keep a log to track patterns and make necessary adjustments.
- Use a continuous glucose monitor (CGM) for real-time insights.
4. Manage Stress
- Chronic stress can raise blood sugar levels.
- Try meditation, deep breathing, or yoga to stay calm.
- Engage in hobbies or activities that help you relax.
5. Get Enough Sleep
- Poor sleep can affect insulin sensitivity.
- Aim for 7–9 hours of quality sleep per night.
- Maintain a regular bedtime routine and avoid screens before bed.
6. Take Medications as Prescribed
- If you have diabetes, follow your doctor’s advice on medications and insulin.
- Never skip doses without medical guidance.
- Work with your healthcare provider to adjust medication if needed.
Final Thoughts
Keeping your blood sugar levels in check is key to maintaining good health. Whether you’re managing diabetes or simply aiming for better well-being, understanding how diet, exercise, stress, and sleep affect your glucose levels can make a big difference. By making smart lifestyle choices, regularly monitoring your blood sugar, and working with your doctor when needed, you can stay in control and prevent complications.
Do you have questions or personal experiences with managing blood sugar? Share your thoughts in the comments below—we’d love to hear from you!

