Living with diabetes doesn’t mean you have to give up on being active. In fact, regular exercise can help you manage your blood sugar, boost energy, and improve your mood. It also lowers the risk of heart disease, helps with weight control, and can even improve how your body uses insulin. But if you have diabetes—whether it’s type 1 or type 2—you need to take extra care to stay safe while working out.
That means planning ahead, checking your blood sugar before and after exercise, and knowing the signs of low or high blood sugar. With the right steps, you can enjoy the many health benefits of staying active without putting your body at risk.
In this post, we’ll walk you through the benefits of exercise for people with diabetes, how to prepare for workouts, and smart tips to avoid risks like low blood sugar. You’ll learn why staying active is one of the best tools for managing diabetes and how to create a routine that works for your body.
We’ll also cover what to eat before and after exercise, how to check your blood sugar safely, and which types of workouts are best. Let’s make your fitness journey safe, effective, and enjoyable—so you can stay strong, healthy, and in control.

Why Exercise Is Important for People with Diabetes
Exercise is a powerful tool in diabetes care. It helps your body use insulin better and lowers blood sugar naturally. When you move your body, your muscles use glucose for energy, which helps bring your blood sugar levels down. Physical activity also improves heart health, strengthens muscles, and can help with weight management. Staying active may also lower blood pressure and improve cholesterol levels.
Over time, regular exercise can reduce the risk of complications linked to diabetes, such as nerve damage and poor circulation. Even small amounts of daily movement can make a big difference in how you feel and how well you manage your condition.
Key Benefits of Exercise for Diabetes:
- Lowers blood glucose levels
- Increases insulin sensitivity
- Supports healthy weight loss
- Reduces risk of heart disease
- Boosts mental health and energy
According to the American Diabetes Association, adults with diabetes should aim for at least 150 minutes of moderate aerobic activity per week. This includes activities like walking, biking, or swimming.
Get the Green Light from Your Healthcare Team
Before starting any workout plan, talk to your doctor or diabetes care team. They can help you choose safe exercises and adjust your medications if needed. Some workouts may affect your blood sugar more than others, so it’s important to get guidance that fits your health needs.
Your care team can also check for any complications, like nerve damage or heart issues, that might change the type of activity that’s best for you. By working with your doctor, you can build a plan that supports your fitness goals while keeping your diabetes under control.
Ask your doctor:
- What types of exercise are safe for me?
- Do I need to check my blood sugar before or after workouts?
- Should I adjust my insulin or food intake?
Your doctor may also suggest seeing a certified diabetes educator (CDE) or physical therapist to create a personalized plan.
Best Types of Exercise for People with Diabetes
The best workout is the one you enjoy and can stick to. A mix of cardio, strength training, and flexibility exercises works best for managing diabetes.
Top Exercise Options:
1. Aerobic Exercises
- Walking
- Swimming
- Biking
- Dancing
- Low-impact aerobics
2. Strength Training
- Bodyweight exercises (squats, push-ups)
- Resistance bands
- Dumbbells or weight machines
- Twice a week is a good goal
3. Flexibility and Balance
- Stretching
- Yoga or Pilates
- Tai Chi
These help prevent falls and keep joints healthy—especially important if you have nerve damage or arthritis.
Tips for Exercising Safely with Diabetes
Working out with diabetes can be safe and enjoyable if you follow a few simple rules. Here’s how to stay on track:
1. Check Your Blood Sugar
Monitor your blood glucose before, during, and after workouts—especially if you take insulin. Exercise can cause your blood sugar to drop, sometimes even hours later. Checking your levels helps you stay safe and avoid highs or lows. If your blood sugar is too low before you start, have a small snack to bring it up.
If it’s too high, wait until it comes down before exercising. During long or intense workouts, check your blood sugar halfway through to catch any sudden changes. After you finish, keep an eye on your levels for the next few hours to prevent delayed drops.
- Before exercise: If below 100 mg/dL, eat a small snack.
- During: Carry quick carbs (like glucose tablets or juice) in case of a drop.
- After: Check again to see how your body responds.
Low blood sugar (hypoglycemia) can happen during or after exercise. Symptoms include:
- Shakiness
- Sweating
- Dizziness
- Confusion
If you notice these, stop and treat it right away.
2. Stay Hydrated
Drink water before, during, and after your workout. Staying hydrated helps your body work better and keeps your blood sugar in a healthy range. Dehydration can raise blood sugar levels and make you feel tired faster. It can also lead to muscle cramps, dizziness, or headaches.
If you’re sweating a lot or exercising in hot weather, you may need to drink even more. Keep a water bottle with you and take small sips often. Avoid sugary drinks or energy drinks, as they can spike your blood sugar instead of keeping you hydrated.
3. Wear Proper Shoes
Foot care is crucial for people with diabetes. High blood sugar can reduce blood flow and damage nerves, making it harder to feel injuries. That’s why it’s important to protect your feet during exercise. Choose well-fitting athletic shoes and moisture-wicking socks to prevent blisters, pressure spots, and sweating.
Avoid shoes that are too tight or too loose. Check your feet daily for blisters, cuts, redness, or swelling. Even small wounds can turn into serious problems if left untreated. If you notice anything unusual, tell your doctor right away. Taking care of your feet helps you stay active and avoid complications.
4. Start Slow and Build Up
If you’re new to exercise, start small. You don’t have to do intense workouts right away. Even 10-minute walks can make a big difference in your health and blood sugar control. Short, daily activities help build a habit without putting too much stress on your body. As you get stronger and more comfortable, gradually increase the time and intensity of your workouts.
Add a few more minutes each week, or try new activities like light stretching, biking, or swimming. The key is to listen to your body and move at your own pace. Consistency matters more than speed or intensity.
5. Don’t Skip Meals
Always eat something before you work out, especially if you take insulin or medications that lower blood sugar. Exercising on an empty stomach can cause your blood sugar to drop too low, which may lead to dizziness, shakiness, or even fainting. A small snack with healthy carbs—like a banana, a slice of whole-grain toast, or a handful of crackers—can give you energy and help keep your levels stable.
If your workout is longer or more intense, you may need a bigger snack or a mix of carbs and protein. Talk to your doctor or dietitian to find the best pre-workout snack for your needs.
A balanced pre-workout snack may include:
- A slice of whole grain toast with peanut butter
- A banana with a handful of almonds
- Greek yogurt with berries
Precautions: When to Be Extra Careful
Some people with diabetes face extra health risks. Talk to your doctor if you have:
- Nerve damage (neuropathy): Avoid high-impact activities. Try swimming or biking instead.
- Eye problems (retinopathy): Skip heavy lifting or jarring movements.
- Kidney disease: Check with your care team for safe activity levels.
Also avoid exercising during peak insulin activity, unless advised otherwise. This can increase your risk of low blood sugar.
Special Considerations for Type 1 Diabetes
People with type 1 diabetes must take special care when exercising because they rely on insulin.
Tips for Type 1:
- Always carry a fast-acting carb source
- Avoid late-night workouts to reduce the risk of overnight lows
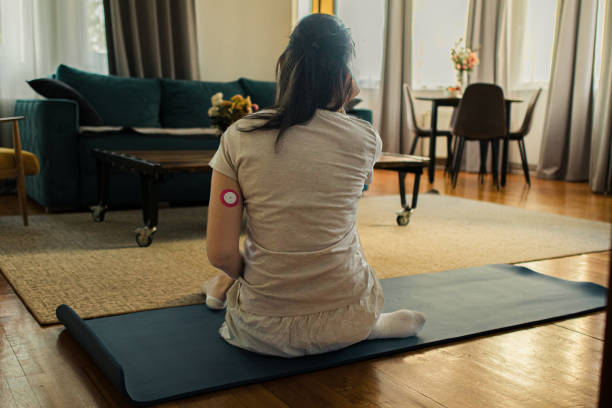
- Use a Continuous Glucose Monitor (CGM) or check levels often
- Adjust insulin based on activity—ask your doctor for help
For more, see this guide from JDRF on Type 1 Diabetes and Exercise.
Sample Workout Plan for Beginners
Here’s a simple weekly plan to get you moving safely:
| Day | Activity |
|---|---|
| Monday | 30-minute brisk walk |
| Tuesday | Light strength training (bodyweight) |
| Wednesday | Rest or stretching/yoga |
| Thursday | 30-minute bike ride |
| Friday | Strength training (resistance bands) |
| Saturday | 20-minute dance workout |
| Sunday | Rest or gentle walk |
Adjust as needed based on how you feel and your doctor’s advice.

What to Keep in Your Diabetes Workout Kit
Always carry these with you:
- Blood glucose meter or CGM
- Fast-acting carbs (like glucose tablets or juice)
- Water bottle
- ID or medical bracelet
- Cell phone for emergencies
- Snacks (protein bar or trail mix)
Call to Action: Take the First Step Today!
You don’t have to become a marathon runner overnight. The first step could be as simple as a walk around the block. Regular movement helps control your blood sugar and boosts your well-being. Start slow, stay consistent, and listen to your body.
👉 Ready to move more with confidence? Talk to your doctor today and make a simple plan. You’ve got this!
Conclusion: Let’s Move Toward Better Health—Together
Living with diabetes doesn’t mean putting life on pause. You can still enjoy the things you love while staying active and healthy. With the right steps, exercise can be a safe and powerful part of your daily routine. It helps you take control of your health and feel more confident in your body.
Whether you’re walking your dog, stretching in the living room, or hitting the gym, your effort matters. Every bit of movement counts—even small steps lead to big results over time. Staying consistent and making activity a habit can improve your mood, energy, and blood sugar levels.
💬 We’d love to hear from you!
What’s your favorite way to stay active with diabetes? Leave a comment below and share your journey. Let’s support each other every step of the way.

