Diabetes is more than just a condition that affects blood sugar levels—it’s a chronic disease that can cause widespread changes throughout your body. Over time, high blood sugar can damage vital organs, nerves, and blood vessels, increasing the risk of serious complications such as heart disease, kidney failure, nerve damage, and vision loss. These effects can impact your quality of life, making it essential to stay informed and take proactive steps in managing your health.
The good news is that with proper care and lifestyle adjustments, many of these complications can be prevented or managed. In this post, we’ll explore how diabetes affects different parts of the body, common symptoms to watch for, and practical tips to help you stay healthy and reduce your risk of complications.
1. Heart and Blood Vessels
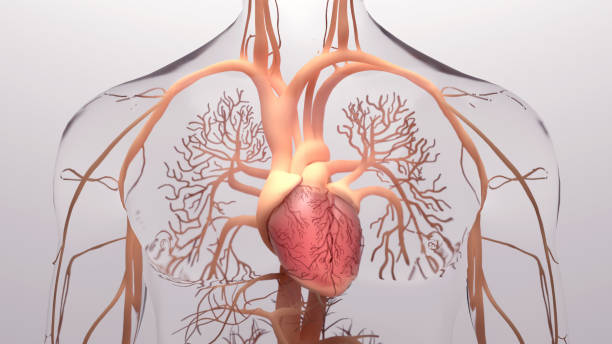
Diabetes significantly increases the risk of heart disease by damaging blood vessels and the nerves that control heart function. Consistently high blood sugar levels can lead to the buildup of fatty deposits in the arteries, reducing blood flow and increasing the likelihood of high blood pressure, heart attacks, and strokes.
People with diabetes are also more prone to developing conditions like high cholesterol and elevated triglycerides, which further contribute to cardiovascular disease.
Key Points:
✅ Increases cholesterol and triglyceride levels – This can lead to clogged arteries, raising the risk of heart attacks and strokes.
✅ Raises blood pressure – Excess strain on the heart can lead to long-term damage and cardiovascular complications.
✅ Prevention is key – Managing blood sugar, following a heart-healthy diet, exercising regularly, and monitoring blood pressure can help protect your heart.
2. Nervous System and Nerve Damage
Diabetes can cause nerve damage, known as diabetic neuropathy, which affects millions of people. High blood sugar levels can gradually harm nerves throughout the body, especially in the legs and feet. This can lead to pain, tingling, numbness, or loss of sensation, increasing the risk of unnoticed injuries, infections, and even severe complications like foot ulcers. If left unmanaged, nerve damage can impact mobility and quality of life.
Key Points:
✅ Common symptoms – Tingling, burning, numbness, or sharp pain, especially in the hands and feet.
✅ Increased risk of injury – Reduced sensation makes it harder to detect wounds, which can lead to infections or ulcers.
✅ Prevention matters – Controlling blood sugar, maintaining a healthy diet, exercising, and regular foot care can help prevent or slow nerve damage.
3. Kidneys
Your kidneys play a crucial role in filtering waste and excess fluids from your blood. However, high blood sugar from diabetes puts extra strain on these vital organs, leading to kidney damage—a condition known as diabetic nephropathy. Over time, this damage can cause protein leakage, reduced kidney function, and even kidney failure if left untreated. Because kidney disease often develops silently, symptoms may not appear until significant damage has already occurred.
Key Points:
✅ Early signs are hard to detect – Kidney disease progresses slowly, and symptoms may not be noticeable until the condition is advanced.
✅ Severe cases may require treatment – If kidney function declines too much, dialysis or a kidney transplant may be necessary.
✅ Prevention and protection are key – Managing blood sugar, keeping blood pressure in check, staying hydrated, and attending regular kidney function check-ups can help safeguard kidney health.
4. Eyes
Diabetes can have a serious impact on your eye health, increasing the risk of vision problems and even blindness. High blood sugar can damage the tiny blood vessels in the retina, leading to diabetic retinopathy—a progressive eye condition that affects millions of people with diabetes. Over time, this damage can cause leakage, swelling, and abnormal blood vessel growth, leading to vision impairment or, in severe cases, blindness.
Key Points:
✅ Early symptoms may include – Blurred vision, floaters, dark spots, or difficulty seeing at night.
✅ Without treatment, vision loss is possible – Advanced diabetic retinopathy can cause permanent blindness if left unmanaged.
✅ Prevention is key – Annual eye exams, blood sugar control, and healthy lifestyle choices can help detect problems early and protect vision.
5. Skin
Your skin is the body’s first line of defense, but diabetes can make it more prone to dryness, infections, and slow healing wounds. High blood sugar levels can reduce circulation and nerve function, leading to dry, cracked skin and an increased risk of bacterial and fungal infections. Skin conditions like diabetic dermopathy, acanthosis nigricans, and ulcers are also more common in people with diabetes. Proper skin care and blood sugar management can help prevent these complications.
Key Points:
✅ Watch for early signs – Dark patches (acanthosis nigricans), sores, frequent itching, or fungal infections.
✅ Hydration and hygiene matter – Moisturizing daily, keeping skin clean, and treating wounds quickly can help prevent infections.
✅ Blood sugar control is essential – Maintaining stable glucose levels supports healthy skin and faster healing.
6. Digestive System

Diabetes doesn’t just affect blood sugar—it can also disrupt digestion and how your body processes food. High blood sugar can damage the nerves controlling the stomach, leading to gastroparesis, a condition that slows stomach emptying. This can cause bloating, nausea, heartburn, and unpredictable blood sugar levels, making diabetes management even more challenging.
Key Points:
✅ Common symptoms – Bloating, nausea, vomiting, heartburn, or feeling full after just a few bites.
✅ Diet adjustments can help – Eating small, frequent meals and avoiding high-fat or high-fiber foods may improve digestion.
✅ Consult your doctor – Medications, dietary changes, and blood sugar management strategies can help ease symptoms and improve digestion.
7. Immune System
Diabetes can weaken your immune system, making it harder for your body to fight off infections and heal properly. High blood sugar levels can interfere with white blood cell function, which is essential for immune defense. As a result, people with diabetes are more prone to bacterial, viral, and fungal infections, including urinary tract infections, pneumonia, and slow-healing wounds. A strong immune system is crucial for maintaining overall health, especially for individuals managing diabetes.
Key Points:
✅ Higher risk of illness – People with diabetes may get sick more often and take longer to recover from infections.
✅ Blood sugar control is key – Keeping glucose levels stable supports a stronger immune response and faster healing.
✅ Prevention matters – Stay up to date on vaccinations, practice good hygiene, eat a balanced diet, and get enough rest to help boost immunity.
8. Mental Health
Living with diabetes can be mentally and emotionally challenging. The constant need to monitor blood sugar levels, manage medications, and follow a strict diet can lead to stress, anxiety, and even depression. Studies show that individuals with diabetes are at a higher risk of mental health conditions, which can, in turn, make diabetes management more difficult. Prioritizing mental well-being is just as important as maintaining physical health.
Key Points:
✅ Increased risk of anxiety and depression – The daily demands of diabetes management can lead to emotional burnout and mental health struggles.
✅ Seeking support is important – Talking to a counselor, therapist, or joining a diabetes support group can provide emotional relief and practical advice.
✅ Lifestyle choices can help – Regular physical activity, healthy eating, mindfulness practices, and good sleep habits can improve mood and reduce stress.
Conclusion
Understanding how diabetes affects your body is key to effective management and long-term health. This condition can impact multiple systems, from your heart and kidneys to your nerves, skin, and mental well-being. However, with the right approach, you can minimize complications and maintain a good quality of life.
By keeping blood sugar levels stable, eating a balanced diet, staying physically active, managing stress, and scheduling regular check-ups, you can take control of your health. Early detection and proactive care make a significant difference in preventing or slowing down diabetes-related complications.
Diabetes may require lifelong management, but with knowledge, support, and healthy habits, you can lead a full and active life while reducing health risks.

