What Is Insulin Resistance?
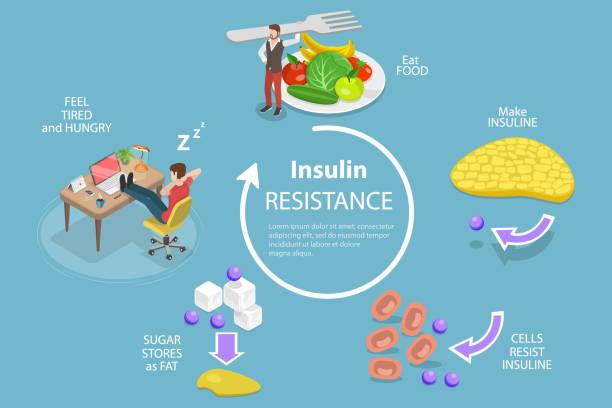
Insulin resistance occurs when the body’s cells no longer respond effectively to insulin, a crucial hormone responsible for regulating blood sugar levels. Normally, insulin helps transport glucose from the bloodstream into cells, where it is used for energy. However, when cells become resistant, the pancreas compensates by producing more insulin to maintain normal blood sugar levels.
Over time, this increased demand can lead to elevated blood sugar levels, increasing the risk of serious health conditions such as type 2 diabetes, heart disease, and metabolic syndrome. Understanding insulin resistance is key to preventing these complications and maintaining overall health.

Causes of Insulin Resistance
Insulin resistance develops due to a combination of lifestyle, genetic, and hormonal factors. Understanding these underlying causes can help in taking proactive steps to improve insulin sensitivity and prevent long-term health issues.
1. Poor Diet
Eating a diet high in processed foods, added sugars, and unhealthy fats can contribute to insulin resistance. Consuming refined carbohydrates—such as white bread, sugary cereals, and pastries—causes frequent blood sugar spikes, forcing the body to produce excess insulin. Over time, this can lead to insulin resistance and an increased risk of type 2 diabetes.
2. Lack of Physical Activity
A sedentary lifestyle reduces the body’s ability to use insulin effectively. Regular exercise, including both cardio and strength training, helps muscles absorb glucose more efficiently, reducing insulin resistance and promoting overall metabolic health.
3. Excess Weight and Abdominal Fat
Being overweight or obese, particularly with excess belly fat, is strongly linked to insulin resistance. Visceral fat, which surrounds internal organs, releases inflammatory compounds that interfere with insulin signaling, making it harder for cells to respond properly.
4. Genetics and Family History
A family history of diabetes can increase the likelihood of developing insulin resistance. While genetics play a role, lifestyle choices such as diet and exercise can help manage the risk.
5. Hormonal Imbalances
Certain health conditions, such as polycystic ovary syndrome (PCOS) and hypothyroidism, can disrupt hormone levels and lead to insulin resistance. Managing these conditions with medical guidance and lifestyle changes can improve insulin function.
6. Chronic Stress
Long-term stress increases the production of cortisol, a hormone that raises blood sugar levels and reduces insulin sensitivity. Practicing stress-reducing activities like meditation, deep breathing, and exercise can help maintain balanced blood sugar levels.
7. Poor Sleep Habits
Not getting enough quality sleep can disrupt metabolism and increase the risk of insulin resistance. Studies show that sleep deprivation affects hormone levels, leading to increased hunger, weight gain, and poor blood sugar control. Prioritizing 7–9 hours of restful sleep each night can support metabolic health.
By addressing these risk factors through healthy eating, regular exercise, stress management, and quality sleep, you can take proactive steps to reduce insulin resistance and improve overall well-being.
Symptoms of Insulin Resistance
Insulin resistance often develops silently, without obvious symptoms in its early stages. However, as the condition progresses, some warning signs may appear, including:
- Persistent fatigue, even after getting enough sleep
- Increased hunger and cravings, particularly for sugary or high-carb foods
- Unexplained weight gain, especially around the abdomen
- Darkened skin patches in areas like the neck, armpits, or groin (a condition called acanthosis nigricans)
- Elevated blood sugar levels, which can lead to prediabetes or type 2 diabetes
- High blood pressure and abnormal cholesterol levels, raising the risk of heart disease
- Frequent urination and excessive thirst, potential indicators of worsening blood sugar control
Recognizing these symptoms early can help in taking proactive steps to improve insulin sensitivity through lifestyle changes like a balanced diet, regular exercise, and weight management. If you notice these signs, consult a healthcare professional for further evaluation and guidance.
How to Reduce Insulin Resistance
Making healthy lifestyle changes can improve insulin sensitivity and lower the risk of developing diabetes. Here are some effective strategies:
1. Eat a Balanced Diet
Focus on whole, unprocessed foods such as:
- Lean proteins (chicken, fish, tofu, eggs, legumes)
- Healthy fats (avocados, nuts, seeds, olive oil)
- Fiber-rich vegetables (broccoli, spinach, carrots, bell peppers, kale)
- Whole grains (quinoa, brown rice, oats, whole wheat bread)
- Low-glycemic fruits (berries, apples, pears, citrus fruits) Avoid sugary drinks, white bread, and processed snacks that can cause blood sugar spikes.
2. Exercise Regularly
Physical activity plays a key role in improving insulin sensitivity. Aim for at least 30 minutes of activity most days of the week. Effective exercises include:
- Aerobic activities like walking, jogging, cycling, and swimming
- Strength training to build muscle and improve glucose absorption
- High-intensity interval training (HIIT) to maximize fat burning and insulin sensitivity
- Yoga and stretching to reduce stress and inflammation
3. Maintain a Healthy Weight
Losing even a small amount of weight (5–10% of body weight) can make a big difference in insulin resistance. A combination of healthy eating and regular exercise can support long-term weight management.
4. Manage Stress
Chronic stress increases cortisol levels, which can worsen insulin resistance. Reducing stress through relaxation techniques can help regulate blood sugar levels. Try:
- Meditation or mindfulness practices
- Deep breathing exercises
- Spending time in nature
- Engaging in hobbies or creative activities
5. Get Enough Sleep
Poor sleep can lead to hormone imbalances and increase insulin resistance. Aim for 7–9 hours of sleep per night. Improve sleep quality by:
- Keeping a consistent sleep schedule
- Reducing screen time before bed
- Creating a relaxing bedtime routine
- Avoiding caffeine and heavy meals late at night
6. Stay Hydrated
Drinking plenty of water supports metabolic processes and helps the body regulate blood sugar levels. Reduce intake of sugary and artificially sweetened drinks, which can contribute to insulin resistance.
7. Consider Medical Help
If lifestyle changes are not enough, a doctor may suggest medications or further testing to manage insulin resistance. Common treatments include:
- Metformin – A medication that improves insulin sensitivity and lowers blood sugar levels
- Hormone therapy – For those with conditions like PCOS that impact insulin resistance
- Regular health screenings – Monitoring blood sugar, cholesterol, and blood pressure levels can help detect and prevent complications early

Final Thoughts
Insulin resistance is a significant health concern that can increase the risk of type 2 diabetes, heart disease, and other metabolic disorders. However, with the right lifestyle changes, it is possible to improve insulin sensitivity and support overall well-being. A balanced diet rich in whole foods, regular physical activity, stress management techniques, and quality sleep all play a crucial role in keeping blood sugar levels in check.
By adopting healthier habits, you can reduce your risk of serious health complications and take control of your long-term health. If you notice symptoms of insulin resistance or have concerns about your blood sugar levels, consult a healthcare professional for a personalized plan to manage and prevent further issues. Taking proactive steps today can lead to a healthier future.